Deconstructing prejudices about schizophrenia
On World Schizophrenia Day in March 2024, a key figure on the prevalence of this mental illness in France has been revealed: almost 1% of the population is thought to be affected, or around 660,000 people. But what exactly are we talking about? There are many preconceptions about this illness. With Dr Sleurs, a psychiatrist at the Orgemont clinic (France), let’s try to deconstruct them to better understand the complexity of the factors and symptoms of this illness, which is little known to the general public.
The main prejudices about schizophrenia
The prejudices surrounding schizophrenia are still deeply rooted in people's minds, and the notions of "dangerousness", "unpredictability" and "irresponsibility"1 are frequently associated with this mental disorder. While 83% of French people first associate schizophrenia with danger to others, almost 70% of GPs still share this idea2...
Another common prejudice is to confuse schizophrenia with Dissociative Identity Disorder (DID). However, these are very different mental disorders, IDD being characterised by recurrent amnesia and distinct personality states, whereas schizophrenia has other specific features (see below).
It is also widely accepted that schizophrenics are 'voice-hearers': "Patients themselves are convinced of this, and are surprised when they are diagnosed, they don't hear voices!
Finally, another prejudice concerns the integration of schizophrenics into society: "Many people around me think that schizophrenics are hospitalised for life, in the belief that they cannot have a professional life, Dr Sleurs continues. However, there are several forms of schizophrenia, and some of them are less symptomatic, allowing them to lead a 'virtually' normal life.”

What is schizophrenia?
Schizophrenia is a heterogeneous disorder characterised by major disturbances in the perception of reality and behavioural changes. It manifests itself through a variety of symptoms classified into three main categories: positive symptoms, negative symptoms and symptoms of disorganisation.
Positive syptoms:
Positive symptoms are all the symptoms that are added. On the one hand, there are delusions, i.e. a distorted interpretation of reality, and/or acoustic-verbal or intrapsychic hallucinations, sensory perceptions with no real external stimulus.
Negative symptoms:
In contrast to the positive symptoms, these are "minus" symptoms such as emotional blunting (restriction of affectivity), cognitive problems (attention problems, memory deficits, difficulty constructing a thought process, etc.), social withdrawal and apragmatism. Apragmatism refers to the inability to initiate or carry out actions directed towards a specific goal. This translates into an absence of motivation and a lack of initiative combined with a form of passivity leading to social isolation. Although less visible, these symptoms represent the most disabling part of the disease, are often present in the residual state, even in stabilised patients, and are associated with patients' functional prognosis.
Symptoms of desorganisation:
Disorganisation is more easily observed. Confused thinking and incoherent speech make it difficult to communicate with others: "We can talk about a blockage in thinking and desynchronisation (discordance) in the expression of emotions," the expert stresses.

24 million
people worldwide suffer from schizophrenia, i.e. one person in 300 (WHO)
80%
is the number of cases where symptoms improve as soon as they are treated
6 out of 10
is the number of press articles using the term "schizophrenia" to refer to something other than this pathology
10 to 13 times more
suicides among people with schizophrenia
More than 2 out of 3 people
suffering from psychosis do not receive specialist mental health care (WHO)
Diagnosing schizophrenia: a delicate process
The protean aspect of the illness, its combination of several symptoms that vary from one individual to another, and the absence of symptoms specific to all schizophrenias make them difficult to detect.
"There is no single symptom that is necessary or sufficient to make a diagnosis of schizophrenia, says Dr Sleurs. The symptom that is most present in all patients is cognitive impairment: deficits in attention, mental flexibility and planning are widespread in people with schizophrenia. But they are found in many other illnesses! Conversely, disorganisation, the most distinctive sign of schizophrenia, is not present in all individuals.” Finally, delusional symptoms or hallucinations are not mandatory for diagnosis.
In addition, the progressive nature of the disease means that diagnosis takes longer. The disease generally manifests itself between the ages of 15 and 25. It is now thought that during adolescence, the number of cerebral connections is significantly reduced. The vulnerability, which was already present but had been compensated for by the child's cerebral plasticity, disappears and the symptoms appear. During adolescence, the brain undergoes a major process of cerebral remodeling. In vulnerable individuals, this process leads to the development of the disease.

What role does the environment play in the development of schizophrenia?
Many of us think that schizophrenia is linked to childhood trauma. However, as Dr Sleurs states: "Schizophrenia is much more an endogenous biological illness than an environmental illness. The current scientific consensus defines it as a neurodevelopmental illness. To be precise, it is more of a polygenic disorder involving a set of genes that amplify the risk of developing it. The heritability of the disease is estimated at 70-80%".
This does not mean that people with schizophrenia will necessarily have children who are carriers of the same illness! That would be to confuse two words: heredity and heritability. The first refers to transmission, while the second refers to the genetic variance observed in a population. However, it would be wrong to dismiss external factors. Exogenous factors in schizophrenia include: factors disrupting development in utero and occurring in the first few years of life (infection, exposure to toxic substances, early foetal suffering, etc.). Later, a difficult life course, with psychological or physical abuse or neglect.

Drugs and schizophrenia: a complex relationship
People suffering from schizophrenia are more likely to use addictive substances: tobacco, alcohol, cannabis and other substances. But for Dr Sleurs, this is not a causal relationship, as "you need a cerebral vulnerability at the outset to potentially develop schizophrenia through drug use. The association is probably bidirectional, with a particular liking for these substances linked to the disease, even though their use is detrimental to the stability of symptoms.”
Two priorities for better treatment of schizophrenia
How are patients treated and is there an effective treatment for the different forms of schizophrenia?
The doctor attempts to answer this complex question, pointing out that "there is no cure for schizophrenia. You learn to limit its effects. Antipsychotics designed to regulate dopamine in the brain work well on the positive symptoms but rather poorly on the negative ones. Acting on the latter would be a major challenge for pharmaceutical research".
The other major difficulty is the patient's denial. "When you have schizophrenia, you rarely perceive the illness. Treatment is therefore often stopped. We need to be able to detect the illness earlier without stopping treatment," he stresses.
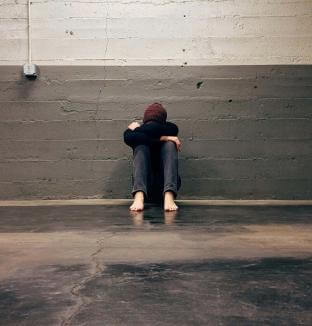
Aside from medical treatment, one of the best ways of supporting people suffering from schizophrenia is to overcome prejudice. As Dr Sleurs puts it: "People suffering from schizophrenia are more likely to be victims of violence than perpetrators. They are victims who, because of their illness and symptoms, are marginalised by others, ostracised and even attacked".
It's a reality that calls for a change in outlook and a collective awakening.

To find out more about this topic...
If you'd like to find out more, take a look at two other articles on the subject of mental health. Enjoy your reading!
[1] Crisp AH, Gelder MG, Rix S, et al. Stigmatisation of people with mental illnesses. Br J Psychiatry 2000 ; 177 : 4-7.
[2] 21es Journées de la Schizophrénie – du 16 au 23 mars 2024.